A non-infectious disease, in which, first of all, the hyaline cartilage of the knee joint suffers, which eventually collapses and stops performing its function, which in turn leads to the destruction of other components of the joint and leads to deformation.
This degenerative-dystrophic disease, as a rule, occurs in women after 40 years, but men can also suffer, especially those who are overweight, exposed to frequent hypothermia, engaged in active sports or as a result of injuries.
Among all arthrosis, gonarthrosis of the knee joint is the most common.
There is an opinion that the cause of gonarthrosis is the deposition of salt in the joints. This opinion is completely wrong and salt deposition is a rather secondary process and causes pain during the development of the disease and is localized at the point of attachment of tendons and ligaments. Prevention plays an important role in disease prevention.
Anatomy of the knee joint
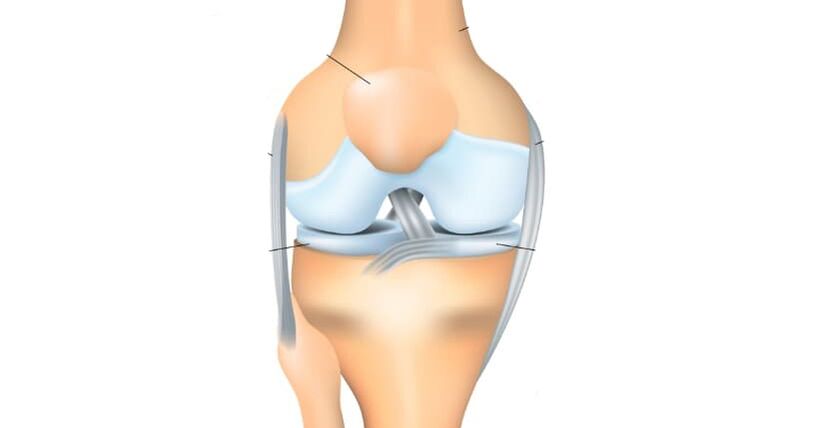
The knee joint consists of two surfaces, formed by the tibia and femur. At the front, the knee joint protects the patella, which moves between the condyles of the femur. The fibula does not take part in the formation of the knee joint and, in principle, does not carry any functional load, for which it is often used to rebuild other bony elements in the body.
All articular surfaces: the tibia, femur and the inner surface of the patella are filled with hyaline cartilage, which is very smooth in texture, has a high degree of strength and elasticity, the thickness of this dense and elastic structure reaches 5-6 mm. Cartilage absorbs the cushion during physical activity, prevents friction and softens the impact.
Classification of gonarthrosis
From the original point of view, gonarthrosis can be classified into primary, manifestation, which occurs without injury and secondary development, which is provoked by trauma, disease or developmental pathology and often occurs as one-sided. In this case, the first type of gonarthrosis, as a rule, occurs in the elderly and is rarely unilateral.
In its development, arthrosis of the knee joint goes through the following stages:
- The first stage of gonarthrosis- does not cause significant suffering to the patient, characterized by intermittent pain or tightening pain, especially after heavy physical exercise, or direct load on the knee joint. The so-called "starting pain" symptom appears, when the patient wakes up suddenly, a painful sensation arises, which gradually disappears, but if an increased load is applied to the limb, the pain returns. There may be some swelling that goes away on its own. Rarely, but it happens, synovitis - fluid accumulates in the articular bag of the knee, because the knee area becomes spherical and swollen, movement in the limb is limited. At this stage, there is no joint deformation.
- Second stage- the patient begins to be disturbed by long and rather severe pains in the anterior part and the inner part of the joint, even with a small load, but after a long rest, they usually disappear. When the joint moves, a buzzing sound is heard, if the patient tries to bend the limb as much as possible, a sharp pain appears. Amplitude in joint movement is limited, and deformation begins to be detected. Synovitis occurs frequently, disturbs for a longer time, continues with a large accumulation of fluid in the joint.
- Third stage- causing great suffering to the patient, constant and disturbing pain not only while walking, but also during rest and even at night, preventing sleep. The joints are already significantly deformed, the position of the limbs becomes X or O-shaped. An undulating gait appears, and often, due to significant deformation, a person cannot just bend, but completely release his legs, as a result of which he has to use crutches or crutchesto walk
Pathology of gonarthrosis of the knee joint

- In the early stages, the first gonarthrosis, due to the development of pathological processes in the vessels that supply the intraosseous hyaline cartilage, the articular surface gradually loses its inherent characteristics. They begin to dry, lose their smooth texture, cracks appear, which cause the sliding of the articular surface to be disturbed, they begin to cling to each other, increasing the defects on the surface. Hyaline cartilage degenerates, losing its shock-absorbing function due to continuous microtrauma.
- In the second stage of gonarthrosis, the degenerative-dystrophic manifestations increase: the joint space narrows, the articular surface is flat, adapting to the increased load. The part of the bone adjacent to the hyaline cartilage of the joint becomes denser, and osteophytes appear along its edges, in the form of growths of bone tissue resembling the shape of spikes. The knee joint capsule also undergoes changes, losing its elasticity. The fluid inside the joint becomes thicker and more viscous, changing its nutritional and lubricating properties, which further affects joint function. Due to malnutrition, the condition of hyaline cartilage worsens, it begins to disintegrate, and in some places it disappears completely. As a result of increased friction, the degeneration of the knee joint increases, which leads to the third stage of gonarthrosis.
- In the third stage of gonarthrosis, a clear limitation of the range of motion in the joint occurs. The surface is significantly deformed, hyaline cartilage is practically absent, the bones seem to be pressed against each other.
Reasons for the development of gonarthrosis
In principle, it is impossible to determine any one cause of gonarthrosis. Basically, its occurrence is due to a combination of several reasons and various internal and external factors.
In 20-30% of cases, gonarthrosis is provoked by traumatic injuries of the knee joint or its components (ligaments, tendons, menisci), as well as fractures of the femur or tibia. The disease manifests, as a rule, 3-5 years after the injury. But there are cases of the development of gonarthrosis in the initial period (2-3 months).
In some patients, gonarthrosis can be triggered by high physical exertion. Often, active physical activity can trigger diseases, especially after 40 years, when people begin to actively exercise to maintain health and realize the need for a healthy lifestyle. Most importantly, the load on the joints is when running, as well as jumping and squatting.
Excess body weight can also cause gonarthrosis, especially in combination with varicose veins on the lower legs. The load on the knee joint increases, and microtraumas or severe injuries of the menisci or ligament apparatus of the joint occur. In this case, healing is more difficult, because. it is impossible to lose weight quickly to lighten the load on the joints.
Various types of arthritis (gouty, psoriatic, rheumatoid, reactive or Bechterew's disease), some neurological pathologies (spinal injury, craniocerebral injury and other diseases that occur with lower limb conservation disorders), as well as hereditary diseases, can trigger the development of gonarthrosis. causing weakness of the connective tissue.
Diagnosis of gonarthrosis
For a patient diagnosed with gonarthrosis, a combination of collecting complaints, examination, and x-ray study is necessary.
Today, the X-ray image of the joint is the simplest and most accessible research method, with the possible help to diagnose patients with a sufficient degree of accuracy, observe the development of the process in dynamics and determine further treatment tactics. Among other things, radiographs allow you to make different diagnoses, for example, to exclude a tumor process in the tissue of the femur or lower leg or inflammation. Also, for the diagnosis of gonarthrosis, computed tomography and magnetic resonance imaging are used, which can show changes not only in the bone structure, but also in soft tissue.
In old age, everyone has certain signs of gonarthrosis, so the diagnosis can only be made after a complete collection of anamnestic data, complaints and visual examination, as well as instrumental research methods.
Treatment of gonarthrosis of the knee joint
When the first signs of knee joint disease appear, it is necessary to consult an orthopedic doctor as soon as possible. At the initial stage of the process, the doctor prescribes drug therapy and the rest of the affected limb.
After the acute period subsides, it is possible to appoint:
- exercise therapy course,
- massage,
- as well as physiotherapy procedures (electrophoresis with analgesics, UHF therapy, magnetic or laser therapy, phonophoresis with anti-inflammatory steroids, mud treatment, etc. )
At the next stage of treatment, the doctor may prescribe drug therapy, which involves taking chondroprotectors that stimulate metabolic processes in the joints. Sometimes intra-articular injections with drugs containing hormones are required. If the patient has the opportunity to receive sanatorium-and-spa treatment, it is recommended to him. Often, to unload the joints, patients are recommended to use crutches when walking. You can use special orthopedic insoles or orthoses for prevention.
If the patient is diagnosed with the third degree of gonarthrosis, where the manifestations are most pronounced (pain, disruption or complete lack of joint function), surgical treatment may be required, which consists of knee arthroplasty. Recovery measures until joint function is fully restored, as a rule, take from 3 to 6 months, after which the patient can return to normal life.
Prevention
To prevent degenerative-destructive changes in the knee joint with age, it is necessary to use physical education, wear orthopedic shoes, control body weight, and monitor rest and exercise regimen.



















